If your child has a cough that just won’t go away after a cold, or if they seem unusually winded after playing at Riverfront Park, you might feel a growing sense of worry. Many Spokane parents find themselves up at 2:00 AM listening to a child’s tight, rattling breath, wondering if this is just a stubborn winter virus or something more serious. It is exhausting to watch your little one struggle for air, and even more frustrating when you aren’t sure how to help them.
Pediatric asthma is a common but manageable condition where the airways become inflamed and narrow, and getting a clear diagnosis is the first step toward a more active, worry-free life. At Mt. Spokane Pediatrics, we focus on moving you from the stress of reactive care to a steady, proactive plan. Our goal is to ensure that your child’s breathing never keeps them from the playground or a good night’s sleep.
What is Pediatric Asthma?
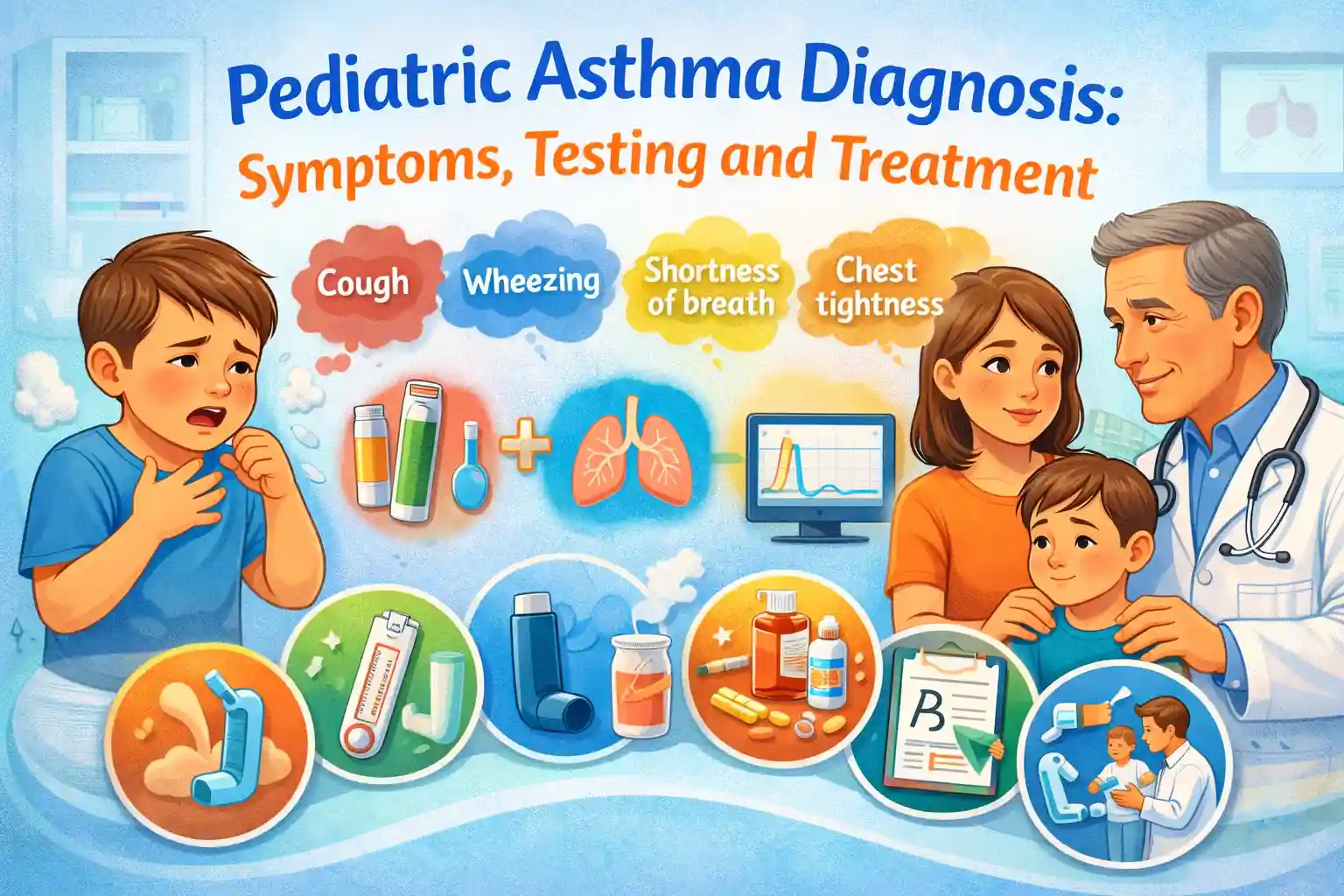
Pediatric asthma is a chronic respiratory condition that affects the airways in a child’s lungs, making it difficult for them to breathe. Asthma causes inflammation and narrowing of the airways, leading to symptoms like coughing, wheezing, shortness of breath, and chest tightness. It can occur at any age, but it often begins in early childhood.
Asthma is one of the most common chronic diseases among children. According to the Centers for Disease Control and Prevention (CDC), approximately 1 in 12 children in the U.S. are affected by asthma. This makes it a leading cause of missed school days and emergency room visits. In Spokane, as in other parts of the country, asthma remains a major concern, especially during allergy seasons or in areas with poor air quality.
Risk Factors for Pediatric Asthma
While the exact cause of asthma is not known, several factors can increase a child’s risk of developing asthma, including:
- Family history of asthma or allergies: Children with parents who have asthma or other allergic conditions are more likely to develop asthma.
- Environmental exposures: Exposure to allergens like pollen, mold, pet dander, and dust mites can trigger asthma symptoms. Air pollution and secondhand smoke are also significant contributors.
- Respiratory infections in early childhood: Viral infections like the flu or respiratory syncytial virus (RSV) can contribute to the development of asthma.
Understanding these risk factors can help parents take preventive measures and manage asthma effectively if diagnosed early.
Symptoms of Pediatric Asthma: How to Spot the Signs
Common Symptoms
Pediatric asthma symptoms vary from child to child, but the most common signs include:
- Wheezing: This is a high-pitched whistling sound when the child breathes out, often a sign of narrowed airways.
- Coughing: Persistent coughing, especially at night or during physical activity, is a common symptom of asthma.
- Shortness of breath: Difficulty breathing, especially after physical exertion or at night, is a hallmark of asthma.
- Chest tightness: A sensation of pressure or tightness in the chest, often described as feeling like something is sitting on the chest.
Asthma symptoms may worsen at night or during exercise, making it harder for children to sleep or engage in physical activities. These symptoms can range from mild to severe, and the frequency and intensity often change over time.
Asthma Attacks and Exacerbations
In some cases, asthma symptoms may suddenly worsen, leading to an asthma attack. During an attack, the airways become more inflamed and constricted, causing extreme difficulty breathing, excessive coughing, and wheezing. Asthma attacks can be triggered by a variety of factors, such as exposure to allergens, viral infections, or even stress.
It’s essential for parents to recognize the signs of an asthma attack early so they can take appropriate action. Signs that asthma are worsening include:
- Increasing difficulty breathing
- More frequent or intense coughing
- Difficulty speaking or playing due to shortness of breath
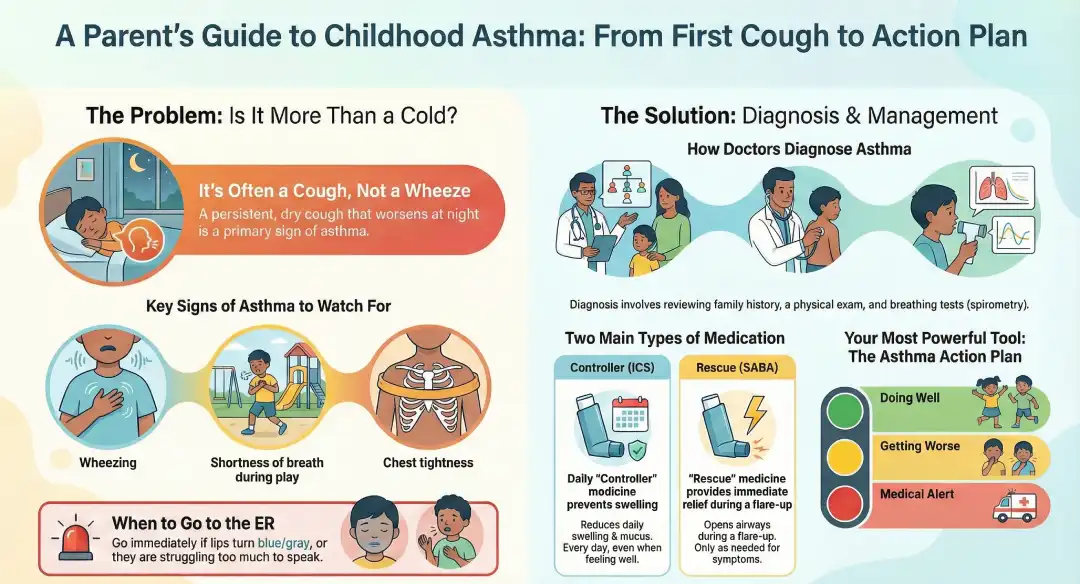
Is It Just a Cold or Childhood Asthma?
In the Inland Northwest, where seasonal shifts and wood-smoke inversions are common, it can be hard to tell a simple chest cold from the beginning of a chronic condition. Asthma is essentially an over-reaction of the immune system that causes the airways to swell and produce extra mucus. While a cold usually resolves in a week or two, an asthma-related cough tends to linger or return every time the weather changes or your child catches a sniffle. At Mt. Spokane Pediatrics, we see asthma as a manageable wiring difference in the lungs. Identifying it early means we can stop the cycle of inflammation before it causes long-term changes to your child’s breathing capacity.
Beyond the Wheeze: The Real Symptoms of Pediatric Asthma
Most people think of asthma as a loud, whistling sound when a child breathes out, but it often shows up in much quieter ways. A chronic, dry hacking cough that peaks at night is one of the most frequent signs we see in our Spokane clinics. You might also notice your child is more tired than usual or complains that their chest feels funny during physical education class. A key sign to watch for is retractions, where the skin pulls in tightly around the ribs or the base of the throat because the baby or child is working extra hard to move air. If your child seems to recover more slowly from respiratory viruses than their peers, it is a significant signal that their airways are more sensitive than average. If your child is experiencing a chronic nighttime cough or visible retractions, scheduling a pediatric acute care visit is essential to determine if these are signs of underlying airway inflammation
Pediatric Asthma Diagnosis: Challenges for Younger Children
Diagnosing a toddler or preschooler can be tricky because they aren’t yet old enough to follow the instructions for traditional breathing tests. For these children, we rely heavily on their medical history and something called the Atopic March. This is the known link between childhood eczema, food allergies, and the eventual development of asthma. If your child has a history of skin rashes or hay fever, their risk for asthma is higher. Often, we will perform a trial of treatment at our North Spokane or Valley offices. We prescribe a safe, low-dose inhaler for a few weeks to see if the symptoms improve. If the cough or wheeze disappears, it gives us a clear clinical answer that we are dealing with asthma. We often identify the first signs of the ‘Atopic March’ during routine well-child exams, allowing us to monitor children with eczema or allergies more closely for the development of asthma.
Ruling Out the Imposters: GERD, RSV, and Bronchiolitis
Before we confirm a Pediatric Asthma Diagnosis, we must ensure we aren’t actually looking at a different issue. In infants, a virus called RSV can cause bronchiolitis, which looks almost identical to an asthma flare-up but requires different care. Similarly, childhood acid reflux (GERD) can cause a chronic cough because stomach acid irritates the throat and airways. We also check for vocal cord dysfunction, where the vocal cords close when they should open, mimicking the feeling of an asthma attack. By doing a full physical exam and listening to your child’s history, your pediatrician ensures that we are targeting the root cause of the breathing trouble rather than just treating the surface symptoms.
| Symptom Category | What to Look For | Common Triggers in Spokane |
| Airway Sound | High-pitched whistle (Wheezing) | Wildfire smoke, cold winter air |
| The Cough | Dry, nighttime hacking | Dust mites, pet dander |
| Visual Signs | Skin pulling in at ribs (Retractions) | Pollen from Ponderosa Pines |
| Activity Level | Stopping during play to catch breath | Exercise, rapid temperature shifts |
Diagnosing Pediatric Asthma: Tests and Assessments
The process of diagnosing pediatric asthma typically involves a combination of medical history review, physical examination, and specific diagnostic tests. Diagnosing asthma early is important for effective management, so it’s essential to work closely with your pediatrician.
 Health History Review
Health History Review
The first step in diagnosing asthma is often reviewing the child’s health history. This includes:
- Family history of asthma or allergies: Since asthma can run in families, knowing if there is a history of asthma or related conditions like hay fever or eczema is helpful.
- Environmental factors: Exposure to allergens or irritants, such as pet dander, mold, pollen, or secondhand smoke, can trigger asthma symptoms.
- Symptom patterns: The pediatrician will ask about the frequency, timing, and severity of symptoms. If the child has symptoms that worsen at night or after exercise, this may indicate asthma.
Physical Examination
During the physical exam, the pediatrician will listen to your child’s chest with a stethoscope for signs of wheezing or other abnormal sounds. They will also assess the child’s overall health and look for signs of airway obstruction or difficulty breathing.
Diagnostic Tests
- Spirometry (Pulmonary Function Test): This is one of the most common tests used to diagnose asthma. It measures how much air a child can breathe in and out and how quickly they can exhale. The results can help confirm the presence of asthma and assess how well the child’s lungs are functioning.
- Peak Flow Meter: This handheld device measures how well air is moving out of the lungs. Parents can use a peak flow meter at home to monitor their child’s asthma over time, helping to detect early signs of an asthma flare-up before symptoms become severe.
- Allergy Testing: Many children’s asthma is triggered by allergens. Skin prick tests or blood tests (like the IgE test) can help identify potential triggers such as pollen, dust mites, or pet dander.
- Bronchoprovocation Testing: If the diagnosis is still unclear, pediatricians may use this test, where a child inhales a substance that irritates their airways (such as methacholine). This helps identify airway sensitivity.
- Chest X-rays or Blood Tests: These tests are used if a doctor suspects other conditions that may be mimicking asthma symptoms or to rule out other diseases.
Treatment Options for Pediatric Asthma
Once asthma is diagnosed, it is essential to establish an effective treatment plan that focuses on controlling symptoms, preventing asthma attacks, and improving lung function. Asthma treatment typically involves a combination of medications and lifestyle adjustments to ensure your child remains comfortable and able to lead an active life.
Medications for Asthma
Quick-Relief (Rescue) Medications
Quick-relief medications are used during asthma attacks or when a child is experiencing difficulty breathing. These medications provide immediate relief by quickly opening the airways. The most common type of quick-relief medication is short-acting beta-agonists (SABA), such as Albuterol, which relax the muscles around the airways and make it easier for the child to breathe. These medications can be lifesaving during an asthma emergency.
Long-Term Control Medications
Long-term control medications are taken daily to prevent asthma symptoms and reduce inflammation in the airways, ensuring better overall control of the condition. The most common long-term medications include inhaled corticosteroids (ICS), such as Flovent or Pulmicort, which help reduce airway inflammation and prevent asthma attacks. Another option is leukotriene modifiers, like Singulair, which block the effects of leukotrienes (chemicals that cause airway inflammation).
For children with more severe asthma, biologic medications like Xolair or Dupixent may be prescribed. These biologics target specific parts of the immune system that are involved in the asthma process, helping to prevent attacks.
Immunotherapy (Allergy Shots)
If your child’s asthma is triggered by specific allergens, immunotherapy (allergy shots) may be recommended. These shots gradually desensitize the child’s immune system to allergens like pollen, pet dander, or mold, reducing the severity of asthma flare-ups over time.
Inhalers, Spacers, and Nebulizers
Medications for asthma are usually administered through inhalers, spacers, or nebulizers. Inhalers are the most common delivery devices for asthma medications. They allow children to inhale the medication directly into their lungs, where it is needed most. However, using inhalers correctly is essential, and pediatricians often guide parents on how to ensure their child is using it properly to get the full benefit of the medication.
For younger children or those who struggle with inhaler techniques, spacers can be used. A spacer is a device that attaches to the inhaler and helps the child breathe in the medication more effectively. It allows for deeper inhalation, ensuring that the medication reaches the lungs. Nebulizers may also be prescribed for children who have difficulty using inhalers. Nebulizers turn liquid asthma medications into a fine mist that can be inhaled through a mask or mouthpiece, making it easier for younger children to breathe in the medication.
Other Treatment Considerations
In addition to medications, managing asthma triggers is an essential part of treatment. Flu shots play an important role in asthma management. Respiratory infections, such as the flu, can exacerbate asthma symptoms, making vaccinations particularly important for children with asthma. Ensuring your child gets the flu shot every year can help reduce the risk of asthma flare-ups triggered by illness.
Managing asthma triggers at home is equally important. Reducing exposure to common allergens like dust mites, pet dander, and mold is critical. Using air purifiers, ensuring proper ventilation, and avoiding smoking indoors can make a significant difference in minimizing asthma triggers. For children with exercise-induced asthma, it is essential to monitor physical activity levels and ensure that a quick-relief inhaler is available for use before engaging in sports.
| Medication Type | Goal of Treatment | How Often It Is Used |
| Controller (ICS) | Reduces daily swelling/mucus | Every day, even when feeling well |
| Rescue (SABA) | Opens airways during a flare | Only as needed (should be rare) |
| SMART Therapy | Combined control and relief | Daily, with extra puffs for symptoms |
| Biologics | Blocks severe allergic triggers | Scheduled injections (for severe cases) |
When to See Your Spokane Pediatrician vs. the ER
Understanding the difference between a minor flare and a true respiratory emergency can save your child’s life and save you unnecessary trips to the hospital. You should schedule a visit at Mt. Spokane Pediatrics if your child is using their rescue inhaler more than twice a week, waking up at night because of a cough, or if their symptoms are interfering with school. However, some signs require immediate emergency care. If you notice your child’s lips or fingernails turning blue or gray, if they are struggling so hard to breathe that they cannot speak a full sentence, or if you see their nose flaring wide with every breath, call 911 or head to the nearest pediatric ER. These are signs that your child is not getting enough oxygen and needs medical intervention right away.
Creating Your Pediatric Asthma Action Plan
The most powerful tool for keeping your child out of the hospital is a written Asthma Action Plan. This is a simple, color-coded guide we create together during your visit. It is divided into three zones: Green (doing well, no symptoms), Yellow (caution, symptoms starting), and Red (danger, seek help). This plan tells you, and your child’s teachers at Spokane Public Schools, exactly which medicine to give and when. By having this roadmap on your fridge and a copy in the school nurse’s office, you ensure that everyone who cares for your child knows how to handle a flare-up before it becomes an emergency. It takes the guesswork out of management and gives your child a safety net wherever they go.
Frequently Asked Questions
Can a child outgrow asthma?
While some children seem to outgrow their symptoms as their airways physically grow larger, the underlying sensitivity of the lungs usually remains. Many children enter a long period of remission during their teens but may find their asthma returns later in adulthood. The goal of early treatment is to prevent permanent scarring of the lung tissue so their lungs stay as healthy as possible throughout their life.
Is a nebulizer better than an inhaler with a spacer?
For most children, an inhaler used with a spacer is just as effective as a nebulizer, and it is much faster and more portable. Nebulizers are generally reserved for very young infants or for severe attacks where a child cannot take a deep breath on their own.
Are steroid inhalers safe for my child’s growth?
Modern inhaled corticosteroids (ICS) are designed to stay in the lungs and have a very low risk of affecting overall growth, especially when used at the lowest effective dose. The risk of untreated asthma, which can lead to stunted activity and frequent hospital stays, is far greater than the minimal risk from the medication.
Conclusion: Breathing Easier with Expert Support
A Pediatric Asthma Diagnosis is not a limitation; it is the first step toward ensuring your child can lead a full, active life. With the shift to modern treatments like SMART therapy and the use of clear Action Plans, the days of asthma keeping kids on the sidelines are largely over. At Mt. Spokane Pediatrics, we are dedicated to helping Spokane families breathe easier by providing the latest testing, education, and personalized care. Whether your child wants to play competitive sports or just enjoy a quiet night of sleep, our team is here to support every breath they take.
